Today we’d like to introduce you to Liza Fisher.
Hi Liza, please kick things off for us with an introduction to yourself and your story.
My story begins in June 2020. A healthy woman in my 30s, I wasn’t very concerned about my own health when Covid decided to take over the world. I started to feel rundown like maybe I had a possible sinus infection and a couple of days later I woke up feeling like an elephant was sitting on my chest. I struggled to breathe, had body aches, a severe headache with light sensitivity and was congested. I knew that I needed to get tested for Covid. I struggled to find a test in Houston, being that it was the first big wave that had come here, I had a friend in Dallas helping me to find testing. My first test came back negative but a couple of days later I ended up in the ER with tachycardia, fever, hyperventilating and turning blue. A spot on my lung was found and I was diagnosed with pneumonia I was told to go home and if you get like this again call 911. Two days later my PCR test came back positive. I continued to try to get healthcare in the next week. I was turned away from multiple locations, including the one emergency room that I had previously been diagnosed at until I found a hospital that had a Covid unit. I waited in a tented facility in the hospital parking lot for triage.
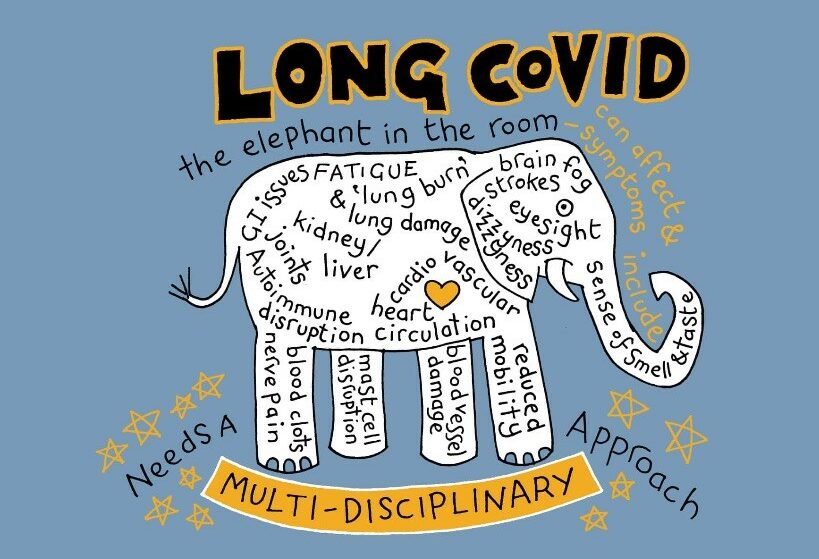
Then was sent for a walk test after waiting several hours I was told I don’t have Covid it’s just a bad flu go home. I told the person that I had tested Covid positive so they asked me what day I was on, to which he said-you’re in the worst of it try to tough it out. Again I was told if you get worse come back and call 911. I had given up on healthcare at that point. Eventually, I found a primary care provider who was accepting Covid positive patients virtually and continued weekly telehealth visits. My symptoms grew from respiratory to gastrointestinal and along the way, neuro crept up. Not getting better my doctor told me to get bloodwork so she could have a better insight although no lab would take me because I hand-tested negative. On July 30 I was told by my doctor to go to an ER and later that day I was admitted into a Covid ICU. Once I don’t remember much in the beginning but I do know that what was shown on TV was real! Once I tested negative I didn’t have to stay in isolation but my hospital visit continued for a week. I was told you’ve passed a point where you could die but now you have lingering symptoms and we don’t know how long they will last. You have Post covered syndrome. I was struggling with mobility and deconditioning, or so we thought, so I was sent to a rehab hospital. I anticipated to stay there for about a week to ten days. I was in that rehab centre for over two months.
Within the first ten days, I developed severe neurological conditions including parkinsonian like body tremors. I lost the ability to walk. The brain fog, which would more accurately be described as a condition similar to a TBI, in which I was performing poorly on Alzheimer’s and dementia tests. Previously Cobalt rehabilitation hospital now Pam had amazing therapists and a wonderful doctor, Dr. Felicity Mack, that helped me along this journey. We continued to try different therapies and medications to treat all of my symptoms but mostly focusing on the mobility. Passing information along to different states my providers found a fabulous management specialist Dr Ankur Khosla. He came up with the idea of implanting a neuromodulation device, a spinal cord stimulator, in my spine to calm down the tremors. A concept similar to what a deep brain stimulator does for Parkinson’s. After struggling to get approval with insurance we did a trial and it was successful to the point where multiple doctors said let’s do it. On October 13, 2020 I went home in a wheelchair with the hope of being able to walk again. It took some time but in November I was able to get my first spinal-cord stimulator implant at T7. After I went back into the rehab hospital for more treatment.
In December I was diagnosed with dysautonomia, a common post-viral condition that Longhaulers are suffering from. During this period the wonderful Dr. Mack got me an appointment with the first post-Covid clinic in the state of Texas. That’s when I was introduced to Dr. Monica Verduzco-Gutiérrez. She validated all that I was experiencing telling me she was hearing the same story from many other Covid/Long Covid patients like myself. She helped me get into TIRR Memorial Hermann and referred me to her former teacher Dr. Cindy Ivanhoe at TIRR brain injury clinic. I began outpatient therapy and continued until I reached a point where my symptoms were prohibiting me from progressing in the spring of 2021. I started to develop what I call my medical team with the quarterback being Dr. Felicity Mack. I knew I was the best person to advocate for my health and my body. I started searching for specialists based off of their research and knowledge of the associated conditions that were being recognized in the long Covid community. I found a POTS cardiologist, a gastroenterologist familiar with dysautonomia, an allergy/immunologist familiar with MCAS, a pulmonologist at Baylor post-Covid clinic and so on and so forth. By the summer of 2021, I had multiple procedures, another spinal implant at C3, a page worth of diagnosis and a pharmacy of daily medication. I was still using the wheelchair. Being fortunate enough to have begun involvement in the Long Covid advocacy community I was connected with researchers and treatments that others have never heard of, An example being EECP Flow Therapy, has been very helpful.
In the beginning, my friends had encouraged me to share what my acute experience was like. I did this by creating Facebook videos. I thought it was only going to be two weeks and little to my knowledge my story sharing in life had just begun. Spring of 2021 I was asked to do a couple of interviews one of which was a PBS podcast. That led to more connections, more interviews and story sharing with Longhaulers, medical professionals and the general public. As my advocacy efforts continued I was asked to share my story before members of Congress at a health subcommittee hearing. Myself and one of my treating physicians, Dr Monica Verduzco Gutiérrez, testified that day about our experiences and to highlight the disability 24-month waiting period for Medicare.
I’m now back in outpatient therapy, have experience symptom improvement or management through multiple interventions and starting to see a clearer picture of my future. Currently, I’m on the board of a couple of nonprofits. I participate in several Covid and Long Covid research projects including the NIH. I’ve been invited to be a co-author as a patient perspective in a Covid-related tremor and internal vibration study. I’ve reviewed and contributed to legislation being brought forth in Congress. I also continue to offer support to fellow Longhaulers and disseminate information with discernment. I now consider myself a full-time patient part-time citizen scientist and my overtime is advocating within the healthcare system. When I was in the hospital I made a video talking about how I’ve been wanting to climb Machu Picchu and I referenced my incentive spirometer as my Machu Picchu. I’ve kept that image in my mind as this entire medical journey has been literally trying to put 1 foot in front of the other climbing my mountain.
Would you say it’s been a smooth road, and if not what are some of the biggest challenges you’ve faced along the way?
This experience has not been smooth although I consider myself very blessed and in a more privileged position than many. I realize very early on that not every doctor was the right doctor for you and it’s OK to discontinue seeing that provider. I also experienced the steep learning curve and that the system is not currently designed to support a complete recovery or as close to as possible. Until having to navigate the complexity of healthcare, insurance, disability and chronic illness I thought they were essentially fail-safe set up. I was disillusioned, unprepared and continue to learn trial by fire. It’s hard enough just being sick the roles you have to play in order to get better are challenging. The biggest struggle I have is the evolving change or shift and identity I experience. Pre-Covid I live a full life of travel activity and independent socialization. Post Covid I’ve become dependent on other people, aware of limitations or capacity and essentially continue to grieve the life I thought I would have.
Appreciate you sharing that. What else should we know about what you do?
The work that I do now is rooted in tenacity compassion and hope. Initially, I want to know to feel as alone as I did in that first month. That transpired to wanting no one to feel dismissed in the healthcare system. Working with support groups and advocacy groups allows one to connect in a time that feels very lonely as well as provide hope. I’m thankful now that I took those videos in the beginning because I can look back and see what progress has been made. That then can be shared with others in order to feel less isolated and believe there may be options and treatments when the majority is not offered them. We all want to be validated in some way in life. Living with what many now know are invisible, chronic and/or post-viral conditions leads to providers and society not believing your lived experience because they can’t see it. In the work that I desire to do, I want people to know that I see them and that their lived experiences are validated. In my overtime work of advocacy, I want to contribute to change support and options. I have a phrase that I continue to repeat and it’s: awareness leads to research leads to treatment, coverage and policy change. What I’m most proud of is simply that I didn’t give up. I didn’t exactly know the path I was taking to climb this mountain of a medical journey but I chose to continue to put 1 foot in front of the other… Even when I physically wasn’t able to I envisioned it in my mind’s eye.
What quality or characteristic do you feel is most important to your success?
I have learned that the concept which has allowed me the most success is mindfulness. Being a Yogi and certified yoga instructor I was familiar with the art of detachment. In this journey, it provided me a way to cope and continue to move forward. I literally had to relinquish control because my body was no longer in my control. In doing so I became detached or unattached from the linear process of recovery I envisioned. So instead of being focused on what I couldn’t do control or the future I became focused on what I could do control and be in the present.
Pricing:
- Donation Fund to help medical bills: https://helphopelive.org/donate-to-campaign/?id=18352
Contact Info:
- Website: LimitlessLiza.com
- Instagram: https://www.instagram.com/limitlessliza2020
- Facebook: https://www.facebook.com/lfisheronu
- Twitter: @LimitlessLiza
- Youtube: https://youtube.com/channel/UCNi6HSlbDCEpePTbweAsQqA